Nitric oxide (NO) has long been considered as a toxic pollutant. In the 90's, Murad, Furchgott, Ignarro, and Moncada showed that it is also involved in vascular relaxation in the human body1-4. NO is a small, diffusible, and transient molecule produced in mammals from the amino acid arginine by three nitric oxide synthase (NOS) enzymes. Low levels of NO produced by the endothelial (eNOS) and neuronal (nNOS) enzymes are crucial for signaling, including vasodilatation, thermoregulation, and neuroprotection. High levels of NO are produced "on-demand" by the inducible (iNOS) enzyme, to help kill tumors, bacteria, and viruses. Both underproduction and overproduction of NO have been linked to various human pathologies. Impaired NO bioavailability from eNOS and nNOS can lead to hypertension, impotence, or atherosclerosis, whereas excess NO production by iNOS can cause inflammation, rheumatoid arthritis, inflammatory bowel disease, immune-type diabetes, stroke, and cancer. The three NOS isozymes are structurally similar and share identical active sites. Thus, targeting iNOS without perturbing the activity of eNOS and nNOS is one of the greatest challenges in the discovery of novel drugs to treat these diseases. Most iNOS inhibitors have not proven successful as drugs, due to negative side effects from high toxicity or poor selectivity.
In this work directed by Elizabeth Getzoff at the Scripps Research Institute (La Jolla, CA), Garcin et al. reveal a new method for the design of selective inhibitors, i.e. those that specifically inhibit one enzyme (in this case iNOS) without limiting the beneficial activities of related enzymes (eNOS and nNOS). This new technique, termed the anchored plasticity approach, should not only provide a general solution for the discovery of treatments for diseases linked to NO overproduction, but also aid the development of drugs against other enzyme families involved in medical conditions including HIV and cancer.
The Getzoff team studied iNOS inhibitors provided by collaborator AstraZeneca. These inhibitors had not yet proven adequate as drug treatments, but some exhibited excellent selectivity for iNOS over eNOS (3000-fold), and reduced pain and inflammation in rodent models of adjuvant-induced arthritis, pancreatitis, neuropathy, and inflammation. Garcin et al. used x-ray crystallography to examine at the atomic level the binding of these inhibitors to iNOS and eNOS, and to determine what features specific to iNOS allowed certain inhibitors to bind more effectively, and thus selectively.
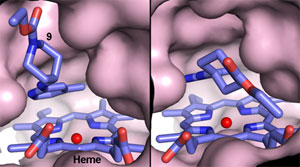
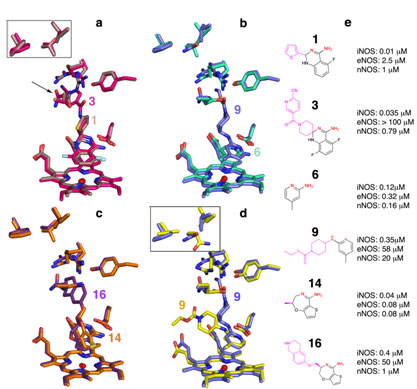
Using data collected at SSRL (and other synchrotrons), they determined seventeen crystal structures of iNOS and eNOS bound to various inhibitors (Fig. 1). All these inhibitors mimic the binding of the arginine substrate in the active site of both iNOS and eNOS. However, for some of these inhibitors, this initial interaction promotes a cascade of subtle conformational changes observed only in iNOS, and ultimately exposes a new binding pocket far away from the active site. These surprising results were tested with more inhibitors, and confirmed by mutagenesis. Effective binding in iNOS depends not only on interactions within the conserved enzyme active site, but also on interactions 20 Å away from the active site, much farther than was suspected. Inhibitors only bind strongly to iNOS to block NO production when they contain a "tail" large enough to bind in this new specificity pocket (Fig. 2; inhibitors 3, 9, and 16). In eNOS, distant residues that are bulkier than those in iNOS prevent the cascade of conformational changes and consequent opening of the new binding pocket, thus resulting in poor inhibitor binding (Fig. 2). Thus, for drug design, the plasticity of distant non-conserved residues can be successfully used to modulate conformational changes of invariant active site residues.
This anchored plasticity approach can be used for the design of selective enzyme inhibitors by incorporating both a core for anchored binding in a conserved active site and extended rigid substituents oriented to exploit protein plasticity far away from the active site. This technique differs from previous inhibitor design methods that focused on differences in residues directly interacting with the inhibitor. These results, obtained with the help of the SSRL beamlines, can be applied to future iNOS inhibitor design for the treatment of inflammation, cancer, and other diseases, while reducing the risks of disrupting the crucial activity of eNOS in maintaining blood pressure.
This work was supported through grants from the U.S. National Institutes of Health and by the Skaggs Institute for Chemical Biology.
- Katsuki, S., Arnold, W., Mittal, C. & Murad, F. Stimulation of guanylate cyclase by sodium nitroprusside, nitroglycerin and nitric oxide in various tissue preparations and comparison to the effects of sodium azide and hydroxylamine. J. Cyclic Nucleotide Res. 3, 23-35 (1977).
- Ignarro, L.J., Buga, G.M., Wood, K.S., Byrns, R.E. & Chaudhuri, G. Endothelium-derived relaxing factor produced and released from artery and vein is nitric oxide. Proc. Natl. Acad. Sci. USA 84, 9265-9269 (1987).
- Khan, M.T. & Furchgott, R. Additional evidence that endothelium-derived relaxing factor is nitric oxide, (Elsevier, Amsterdam, 1987).
- Palmer, R.M.J., Ferrige, A.G. & Moncada, S. Nitric oxide release accounts for the biological activity of endothelium-derived relaxing factor. Nature 327, 524-526 (1987).
Garcin E.D., Arvai, A.S., Rosenfeld R.J., Kroeger, M.D., Crane, B.R., Andersson G., Andrews A., Hamley P.J., Mallinder P.R., Nicholls D.J., St-Gallay S.A., Tinker A.C., Gensmantel N.P., Mete A., Cheshire D.R., Connolly S., Stuehr D.J., Aberg A., Wallace A.V., Tainer J.A., Getzoff E.D. 'Anchored plasticity opens doors for selective inhibitor design in nitric oxide synthase.' Nat. Chem. Biol. 4 (2008), 700-707.




