In a bone-tooth fibrous joint, the articulation between harder materials such as the cementum of the tooth root and alveolar bone (human jaw bone) of the socket is permitted by an intervening softer periodontal ligament. To investigate adaptations of the bony socket, basic principles from tribology, mechanics of materials, and materials science were used to postulate that the ductile nature of an alveolar bone can prompt a reactionary response in root cementum. The common principle in joint mechanics is that loads are distributed with minimum to no stress concentrations when articulation occurs between two congruent surfaces. However, when congruency is disturbed due to bony adaptations or other forms of growth between the articulating surfaces, the resulting stress concentrations can potentiate the joint toward malfunction.
Interestingly, the dynamics between the intervening soft and hard tissues, specifically within the bone-tooth complex, further translates into biologics at the attachment sites and functional interfaces. Tissues and interfaces will continue to adapt to accommodate loads, of physiological or nonphysiological forms (parafunctional loads). Given this doctrine (D.W. Thompson, 1961), the uniquely adapted bone was examined within the bone-ligament-cementum complex of humans. In this study, a specific type of alveolar bone known as bundle bone, commonly found as a result of adaptation due to function and age, was investigated. Hence, this study highlights the lamina dura (adapted alveolar bone that interfaces with the ligament), but interrogates the previously described protrusions (Hurng et al., Biomaterials, 2011) that come off of the lamina dura within the context of joint function. The complexes tested were those removed for orthodontic purposes and were neither periodontally diseased nor affected by dental caries.
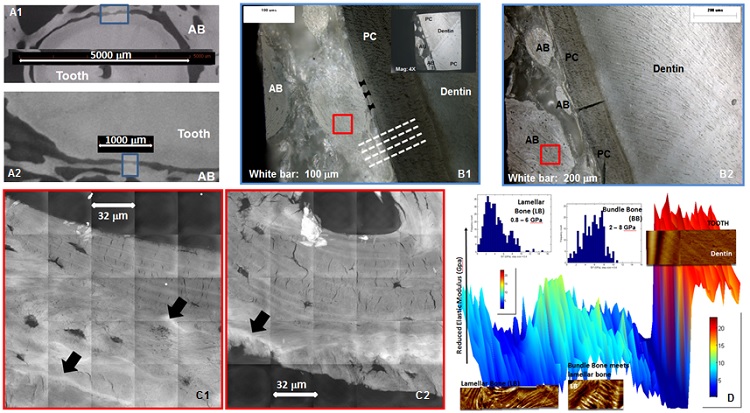
Nanoscale structural properties of the ligament-bone attachment site and interface as revealed by x-ray microscopy at SSRL’s Beam Line 6-2 provided insights into the relationship between functional strain and bone quality. Specifically, bony protrusions or adaptations identified as bundle bone showed structural, biochemical and mechanical heterogeneities that were dissimilar in elemental composition and mechanical properties from lamellar bone (a layer-by-layer structure commonly used to describe bones). X-ray fluorescence imaging of the bony protrusions using SSRL’s Beam Line 2-3 revealed higher concentrations of elemental zinc, calcium and phosphorus as compared to lamellar bone. In addition, the innate resistance of adapted/bundle bone to mechanical load (elastic modulus) was significantly higher than its adjacent lamellar bone (Figure). Based on the results, it is proposed that the observed physicochemical heterogeneities could be the functional cues for an original PDL-bone attachment site to serve as the site of origin for bony protrusions. Additionally, the heterogeneities in physicochemical properties can be considered as discontinuities and could be “markers” indicative of pathological adaptations of alveolar bone. From a joint perspective, the discontinuities can perpetuate functional demands and shift the organ to a pathological regime.
Local functional adaptations can result in unfavorable and poorly understood clinical outcomes such as an increased range of tooth motion or ankylosis of a tooth. Another unfavorable clinical outcome is a decreased range of tooth motion due to bone ingrowth toward the cementum, resulting in a narrowed PDL space and promoting ankylosis (Hurng et al., 2011). Hence, elucidating the adaptive nature that maintains a functional PDL space (Ho et al., 2010) within the bone-tooth complex is essential in: 1) reversing an adaptation before it becomes detrimental; 2) providing proper diagnostics for an appropriate treatment plan; 3) development of therapeutic devices (e.g. braces) for an optimum occlusal function with minimal to no effect on overall joint function. Ultimately, increased clinical success lies in prevention through early intervention of the globally prevalent clinical issues (e.g. malocclusion and periodontal degeneration due to periodontitis potentiated with malocclusion), thereby significantly reducing oral health care costs.
- J. Hurng, M. P. Kurylo, G. W. Marshall, S. M. Webb, M. I. Ryder, and S. P. Ho, "Discontinuities in the Human Bone-PDL-Cementum Complex", Biomaterials 32, 7106 (2011)
- S. P. Ho, M. P. Kurylo, T. K. Fong, S. S. J. Lee, H. D. Wagner, M. I. Ryder, and G. W. Marshall, "The Biomechanical Characteristics of the Bone-Periodontal Ligament-Cementum Complex", Biomaterials 31, 6635 (2010)
- D. P. Mathews and V. G. Kokich, "Accelerating Tooth Movement: The Case against Corticotomy-induced Orthodontics, Counterpoint", Am. J. Orthod. Dentofac. 144, 4 (2013)
- D. W. Thompson, "On Form and Mechanical Efficiency", in On Growth and Form, Cambridge University Press, 1961.
S. P. Ho, M. P. Kurylo, K. Grandfield, J. Hurng, R.-P. Herber, M. I. Ryder, V. Altoe, S. Aloni, J. Feng, S. Webb, G. W. Marshall, D. Curtis, P. Pianetta and J. Andrews Hayter, "The Plastic Nature of the Human Bone-Periodontal Ligament-Tooth Fibrous Joint", Bone 57, 455 (2013), DOI: 10.1016/j.bone.2013.09.007